Chinese Medicine for Diarrhea
- Jul 19, 2022
- 13 min read
Updated: Apr 25, 2025
Written by Eduardo Velasco Valido AP, LAc
Introduction
The WHO has defined diarrhea as having at least three loose stools each night and having more than the average stool size. Acute and chronic are generally grouped by duration. Primarily acute diarrhea is attributed to several factors, while chronic diarrhea is more complex. Acute intestinal tract infections can usually be healed within three days — usually 3 to 4 days. Nevertheless, chronic diarrhea can sometimes last up to three months. Various factors can cause chronic diarrhea. Sadly, many of them have symptoms for no reason.

Diarrhea is considered when the patient is suffering from too frequent passage of loose or watery stools. It produces an increase in softness or fluidity of the stools with an increase in the frequency of the bowel movement.
In our time, diarrhea is still one of the leading causes of infant mortality worldwide.
In Traditional Chinese Medicine TCM, Diarrhea is related to the Spleen, Stomach, and Large Intestine. The Spleen governs the transformation and transportation; the Stomach is in charge of the reception of the food, its decomposition, and sending down the turbid, and the Large Intestine discharges the final waste.
If any of these organs contract an external pathogen, or the patient has an irregular diet, an emotional imbalance, or any other disharmony between organs and viscera, it may inhibit the ability of transformation and absorption of food and liquids and produce obstruction in the transportation, un bearing and down bearing, and lack of separation of the clear and the turbid causing the two to become mixed up and move down the Large Intestine producing diarrhea.
Irritable bowel syndrome
Irritable bowel syndrome is a gastrointestinal disorder commonly attributed to recurrent abdominal pain that occurs in response to changes in digestive patterns. IBS affects about 2 million people worldwide. IBS occurs as mainly diarrhea-dominated IBCs — primarily diarrhea. Pathogenetic is complicated by difficulties in treating.
In Traditional Chinese Medicine, there are 3 main reasons for the origin of Diarrhea:
1.- External pathogen, mostly Damp with or without Heat or Cold. Once the pathogen penetrates the Spleen or Stomach, disturbing the digestive functions.
This type of Diarrhea is usually acute and self-limiting, but if the patient is weak or receives the wrong herbal medicine, treatment can become chronic.
Diarrhea can also be due to Blood stagnation and food stagnation.
2.- Weak function of Spleen; In Chinese medicine, Spleen deficiency is the primary factor, and Dampness is the secondary. This is a chronic situation; this patient tends to suffer from an external pathogen and may complicate the pattern, making it deficient and excess simultaneously.
3.-Liver Qi stagnation produces hypersensitivity and hypertonicity of the gut. The gastrointestinal system suffers a chronic dysfunction due to an overaction from constant emotional stress. This cause is often aggravated with Spleen deficiency because the Liver controls Spleen in the Ko circle. This is the classic irritable bowel syndrome or IBS patients with alternating loose stools and constipation.
ETIOLOGY
External Pathogens
The primary pathogen is always Dampness because it quickly weakens Spleen’s digestive capacity. Once depleted, Spleen will produce more Dampness and create a vicious circle.
In Chinese Medicine, we describe Dampness as heavy and turbid in nature, sinking downward and creating Diarrhea.
The invasion of external pathogens may produce systemic symptoms like fever, chills, and myalgia or may implicate only digestive symptoms.
There are four common types of external pathogenic diarrhea:
DAMP HAT | With external symptoms |
Without external symptom | |
DAMP COLD | With external symptom |
Without external symptoms |
Diet

The food we eat is a fundamental part of patients with diarrhea. Eating spoiled or contaminated food is a common cause of acute diarrhea. In diarrhea, Traditional Chinese Medicine can be described as Summer Heat, Cold, Damp, or Damp Heat.
Regular changes in the diet while traveling easily upset the digestive system promoting diarrhea in some people.
Too much cold or raw food ingested in summer may weaken Spleen Qi and Yang, creating Dampness and Diarrhea. Eating irregularly, missing meals, and eating too late at night also weaken the Spleen Qi and Yang.
Overeating heating foods like chilies, coffee, spirits, and spices can damage the Yin and produce Damp Heat.
Eating in a stressful motion will upset the Spleen and promote the Liver invasion of the Spleen and Stomach, producing Diarrhea.
Dairy products and excessive sugar intake will crate Dampness and Phlegm, producing Diarrhea.
The diet is an important integral part of the treatment of diarrhea.
Emotion
Emotional stress is a common cause; the gastrointestinal system is susceptible to mental or emotional stress. This is often found within the same members of a family. Emotions easily produce irritable bowel syndrome IBS, alternating periods of diarrhea, and constipation.
Anger, resentment, frustration, and stress cause Qi Stagnation which will affect the capacity of the Spleen and Stomach to the digestive system, producing abdominal pain.
Living or working in an emotionally stressful environment will quickly produce an invasion of the Liver, Spleen, and Stomach.
Fighting while eating or watching political news at the table will promote digestive disharmony.
Chronic Liver Qi stagnation will produce Heat which could cause Blood to move recklessly, producing diarrhea with bleeding. Long-term Qi stagnation may also have Blood stagnation and the development of tumors on the intestines.
Excessive worry and overthinking will deplete Spleen Qi and will invade the Liver to invade Spleen, resulting in more damage.
Spleen and Stomach Qi Deficiency
Overwork, excessive worry, irregular diet, no physical activity, or long-time illnesses will damage Spleen Qi and produce bowel disorders.
The spleen governs “the raising of the clear and the descend of the turbid”; if Spleen is too weak, the turbid (Dampness and waste materials) will sink, producing diarrhea.
Patients with long periods of sitting and mentally working like studying or working with computers may weaken the Spleen, especially if this lack of activity is combined with an inappropriate diet.
Spleen and Kidney Yang Deficiency
Spleen Yang can be easily damaged in patients with bad eating habits, and Kidney Yang deficiency may be due to inherited conditions or may be developed by age, overwork for long periods, or in men for excessive ejaculation or in women for having too many pregnancies or for not having time to recover between pregnancies.
The failure of Spleen and Kidney Yang’s fluid metabolism may lead to the accumulation of pathological fluids in different parts of the body, depending on the particular constitution of the patient. The most common is edema, but it may also produce diarrhea.
Blood Stagnation
Usually happens in chronic irritation of the Large Intestine. A chronic liver qi stagnation may easily, with time, produce blood stagnation, or a chronic food stagnation may produce Dampness or Phlegm with Heat which will dry the intestinal walls and inhibit the blood flow producing physical lesions on the intestine. It produces abdominal pain characterized as fixed and stabbing.
Blood stasis may be produced easily by surgery or by a traumatic event.
DIAGNOSIS
The eight principles guide the diagnosis.
The classic patterns of diarrhea may be wind-cold, cold-damp obstructing Spleen, damp-heat, summer-heat-damp, food stagnation, Liver Qi stagnation, Spleen Qi deficiency, Kidney Yang deficiency, etc.
The patterns of diarrhea may be pretty complicated, but when making diagnostic criteria, we focus only on exterior conditions and miscellaneous diseases.
With external conditions, we can always find an excess of the six evils, especially damp heat or damp cold; the six diseases occur considered acutely and suddenly and usually last a short time.
It is fundamental to differentiate between cold and heat. It is considered a cold pattern if the stools are clear, thin, and with a mild odor. It will be regarded as wid-cold diarrhea if it comes with an aversion to cold, fever, and head and body aches. If there is vomiting and sudden abdominal pain, it is considered cold evil. If the color of the stool is yellow, there is a strong smell, and a burning feeling in the anus is viewed as a heat pattern; if there is fatigue of the head and body and abdominal oppression is considered damp-heat diarrhea.
For miscellaneous diarrhea, it is easy to find a history of the wrong diet, overwork, or unhealthy lifestyle. The disease emerges slowly and lasts for an extended period.
In miscellaneous diarrhea, we need to differentiate between excess and deficiency. If there is abdominal pain with pressure and reduced pain after defecating, it will be considered an excess pattern. If there is a history of consuming wrong foods, it would be a pattern of Food Stagnation. If the symptoms come with strong emotions, it would be Liver Qi stagnation. If the problem has been for a long time, the abdominal pain is not severe and feels better with pressure, and a warm temperature indicates a deficiency pattern. If it is Sp Yang deficiency, diarrhea will come with signs of cold from deficiency, and if it is Kidney Yang deficiency, in addition to the cold, the patient will suffer pain in the lumbar area and knees.
Pulse

The correct Pulse Diagnosis is the best way to determine the nature of the problem. If the practitioner has good skills, they can decide on the nature of diarrhea, if it is due to Heat or Cold, Excess or Deficiency, Exterior or Interior, or Yin or Yang.
We can also see if the patient has Dampness, Blood Stasis, Qi Stagnation, lumps, hemorrhoids, irritable bowel syndrome, etc.
The proper Pulse Diagnosis plus the Ear diagnosis is the most accurate Diagnosis, performed by the best Traditional Chinese Medicine doctors. If a practitioner has good training, only the pulse and ear observation are enough to make an accurate, precise diagnosis.
Abdominal palpation
If the practitioner has not had good pulse skills, the palpation of the abdomen can provide precise information that would help to determine the proper syndrome differentiation, avoiding a wrong diagnosis and a wrong treatment, and be able to prescribe the correct Chinese herbs. The palpation of the abdomen can differentiate between excess and deficiency, checking if there is abdominal pain or not, and between cold and heat, which would be essential. Then they would know if the treatment goes towards stimulation of Spleen or towards the elimination of Dampness, cooling or warming, etc.
TREATMENT OF DIARRHEA

In clinical practice, usually, Diarrhea responds very well to Traditional Chinese Medicine treatments. In deficiency and Blood stasis patterns, recovery will require longer times.
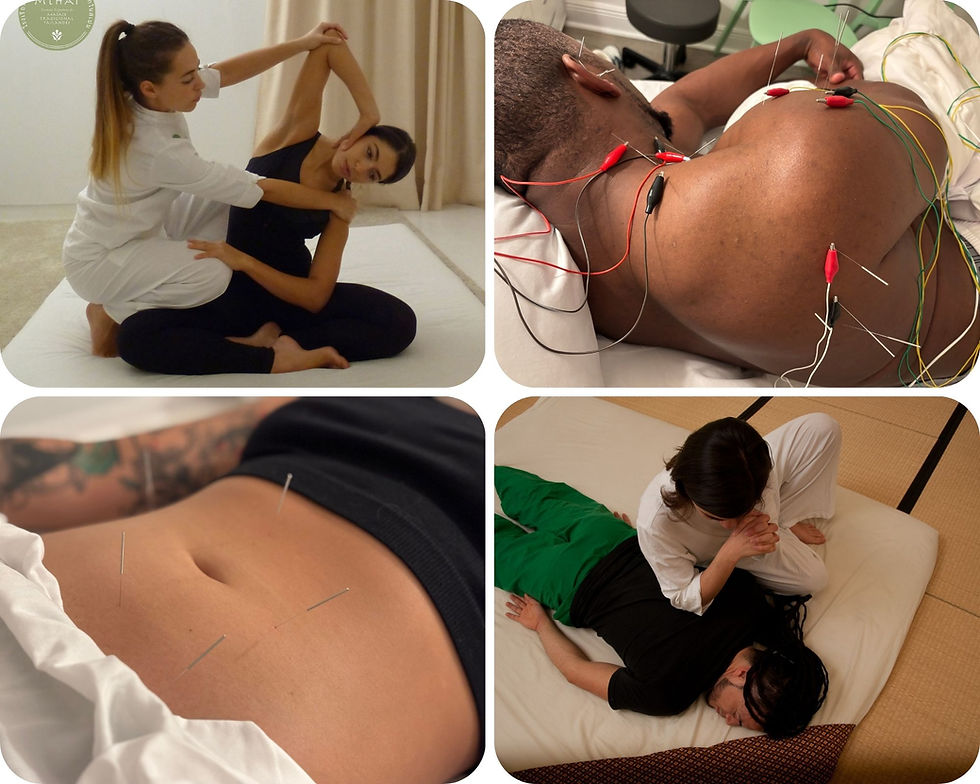
Chinese herbal medicine, acupuncture, and choosing the proper nutrition are the essential tools to help with the treatment.
Cautions and considerations:
If the treatment principle is to expel pathogens, avoid astringent and supplementing herbs.
Overusing bitter and cold Heat clearing herbs may easily damage Spleen and provoke deficiency diarrhea, making the treatment fail.
If the herbalist uses only sweet warming herbs to tonify Spleen, it will produce more Dampness and aggravate the problem.
Proper Diet For Diarrhea:
Foods to Take:
The essential diet during diarrhea should be small meals that are well chewed; that is why congees of rice, barley, or oat are so helpful. Take lots of fluids to counteract possible dehydration. Available remedies for all types of diarrhea include; rice broth, blackberry juice, garlic, leek, eggplant, umeboshi plum, aduki bean, sweet rice, and yam. Also, non-diuretic fluids like lemonade, rice, short-grain (glutinous) rice, millet, blueberries, button or crimini/portobello mushrooms, shredded apple; cooked, warm food.
If there is damp heat, millet porridge, mint, pineapple, eggplant, bamboo sprouts, cucumbers, spinach, mung beans, and dandelion.
If there is Qi and Yang deficiency, dried ginger, nutmeg, fennel, pureed carrots, or crimini/portobello mushrooms, possibly some honey or brown sugar.
Foods to Avoid:
Raw and thermally cool or cold foods (salads, fruit, fruit juices), dairy products, denatured foods, frozen food, and canned food. Honey, spinach, cow's milk, apricot, sesame seeds, oils, and any food that are difficult for the digestive system.
Summer damp or traveler’s diarrhea
SYMPTOMS
- Acute diarrhea with borborygmus, abdominal pain, and cramping. The passage of stools may be urgent and watery.
- Nausea and vomiting
- Heaviness on the head, foggy-head feelings.
- Fullness feeling in the abdomen and possible in the chest
- Lethargy
No sweating
Pulse: floating, soft, tight, or slippery
Tongue: thin or greasy white coat
TREATMENT PRINCIPLE
Clear the exterior and eliminate Dampness
CHINESE HERBAL MEDICINE
HUO XIANG ZHENG QI PIAN or ZHUI FENG SU HE WAN
If the patient has more Heat signs like explosive foul diarrhea, high fever, dark urine, irritability, and rapid pulse use: BAO JI WAN
ACUPUNCTURE TREATMENT:
LI 4: expels pathogens
LI 11: clears Damp-Heat from Yang Ming
St 25: clears Damp Heat and stops Diarrhea
Ren 4: stops diarrhea
Ren 12: harmonizes Stomach
St 37: regulates Stomach and Large Intestine
Sp 9: drains Dampness and Damp-Heat from lower Jiao
Damp Heat
It may be acute or chronic, usually related to food habits.
SYMPTOMS
Dark urine
Irritability
Sweating
Fever or afternoon fever
Urgent, foul smell, burning or itching anus diarrhea.
Pulse: rapid and slippery
Tongue: greasy yellow coat, red tongue
*May be chronic in patients who didn’t get proper treatment, especially when acquired diarrhea in tropical countries.
TREATMENT PRINCIPLES
Stop Diarrhea and clear Damp Heat
CHINESE HERBAL MEDICINE
HUANG LIAN JIE DU WAN
HUANG LIAN SU PIAN
ACUPUNCTURE TREATMENT
St 44: clear Heat from Yang Ming
LI 11: clear Heat from Yang Ming
Sp 90: clear Damp Heat from Lower Jiao
St 37: eliminates Damp Heat from Intestines
St 25: clears Damp Heat and stops Diarrhea
Cold Damp
Usually due to overconsumption of raw and cold foods or after using antibiotics or other cooling medications.
It may be acute or chronic, but it has no exterior symptoms.
SYMPTOMS:
Borborygmus
Nausea
Clear urine
Tiredness and sleepiness
Distending abdomen
Recurrent Diarrhea
Heat reduces the discomfort.
Pulse: slippery
Tongue: Thick, greasy coat
TREATMENT PRINCIPLES
Dry and warm, Cold Damp, and strengthen the Spleen to stop Diarrhea.
CHINESE HERBAL MEDICINE
PING WEI SAN
FU ZI LI ZHONG WAN
ACUPUNCTURE TREATMENT
Sp 9: Promotes urination and eliminates Dampness from Lower Jiao
Sp 6: Strengthens Spleen
St 36: Warms and strengthens Spleen and Stomach
St 37: Eliminates Damp from Intestines
Sp 3: Tonify Spleen
Usually, this kind of diarrhea is straightforward to treat, but the patient must avoid raw, cold, and cooling foods.
Food Stagnation
This case is usually produced by wrong food habits, overeating too often and at bad times, late at night. It usually would have other symptoms like nausea or acid reflux, but when combined with Damp Heat, it may quickly produce diarrhea.
SYMPTOMS
Acid reflux
Nausea
Strong smell gas
Halitosis
Foul Belching
Patients with abdominal pain and distention relieved by diarrhea
Foul diarrhea with or without undigested food.
TREATMENT PRINCIPLES
Eliminate Food Stagnation and strengthen the Spleen
CHINESE HERBAL MEDICINE
BAO HE WAN
JIAN PI WAN
ACUPUNCTURE TREATMENT
Ren 4: Treat indigestion and diarrhea
Ren 12: Clear food stagnation from the Stomach
St 25: Clears food stagnation and stops diarrhea
St 36: Tonify Stomach and Spleen and stops diarrhea
St 37: Eliminates stagnation from Stomach and Large Intestine
St 40: Clears Food Stagnation and Phlegm Stagnation
St 44: Clear Food Stagnation and Heat from Stomach
We must educate the patient, teach them to have better dietary habits, and practice exercise.
Liver Qi Stagnation
The stress from the Liver attack the Intestine and unable the digestion function, reducing the circulation of Qi and Blood in the Large Intestine. In the beginning, the patient will suffer only occasional episodes. Still, if the Liver Qi stagnation gets chronic, the same will happen with bowel habits, producing diarrhea-predominant irritable bowel syndrome in IBS patients.
With time the Qi stagnation may produce Heat that may damage Yin. It also can cause Blood stasis in the Intestines.
SYMPTOMS
Borborygmus
Indigestion
Gas
Hypochondriac tension
Depression, irritability
PMS
Breast tenderness
Shoulder and neck pain
Patients with recurrent diarrhea may be preceded by abdominal pain. Also, diarrhea may be alternated with constipation, IBS, or irritable bowel syndrome.
Pulse: wiry
Tongue: regular, slightly red edges.
TREATMENT PRINCIPLES
Treatment of irritable bowel, harmonize Liver and Spleen, strengthen Spleen and stop diarrhea.
CHINESE HERBAL MEDICINE
CHAI HU SHU GAN WAN
JIA WEI XIAO YAO WAN
ACUPUNCTURE TREATMENT
Liv 3 & Li 4: the four gates move Qi and blood, calm the intestines, and reduce muscle spasms.
Ren 12: regulates Qi in the abdomen
St 25: regulates the intestines
Liv 13: promotes the smooth flow of Liver Qi and helps digestion
St 36: tonify Stomach and Spleen
Sp 6: strengthens Spleen and regulates Liver Qi
Pc 6: spreads Liver Qi
Yin Tang: calms Shen
*If the source of external stress can be resolved, Liver Qi Stagnation Diarrhea has a good prognosis
Spleen and Stomach Qi Xu
This is a typical pattern in people with poor diet habits, which is easy to see in patients with weak digestive systems. The Spleen cannot properly digest the food, making Dampness and undigested foods sink down the intestines, producing Diarrhea.
SYMPTOMS
Patients with frequent diarrhea or loose stools
Aggravated with fatigue
Puffiness around eyes
Pale complexion
Weakness
Weight loss
Symptoms get worse right after eating
TREATMENT PRINCIPLES
Strengthen Spleen, dry Dampness, and stop Diarrhea
CHINESE HERBAL MEDICINE
SHEN LING BAI ZHU WAN
XIANG SHA LIU JUN ZI WAN
ACUPUNCTURE TREATMENT
Ren 12: Tonify Stomach Qi
Ren 4: strengthen digestion
St 25: stop diarrhea and tonify Intestine
St 36: Tonify Spleen and Stomach Qi
Sp 9: drains dampness from Lower Jiao
Sp 6: Tonify Spleen and work in synergy with Sp 9
BL 20: Tonify Spleen
BL 25: Tonify the Large Intestine and stops diarrhea
*With the correct treatment and herbal medicine, patients should see improvements within the first two weeks of treatment, and the problem should be corrected within a few months.
SPLEEN AND KIDNEY AND YANG XU
This is a more severe case than Spleen Qi Xu. The weakness of the Kidney makes it more chronic and more difficult for the patients to respond to the treatment.
SYMPTOMS
Lower back and knee pain or soreness
Fatigue
Poor appetite or anorexia
Abdominal coldness
Aversion to cold
Diarrhea occurs first time in the morning l between 5-7 am
Undigested food in stools
Fecal incontinence
CHINESE HERBAL MEDICINE
LI ZONG WAN
SI SHEN WAN
FU ZI LI ZHONG WAN
ACUPUNCTURE TREATMENT
St 25: Stop diarrhea and improve Large Intestine function
St 36: Tonify Spleen and Yang Ming function
Ren 4: Warms and tonify Kidney
Ren 12: Tonify Stomach
Sp 6: Tonify Spleen and Kidney at the same time
Du 4: Warms Kidney Yang (better with moxa)
Du 20: Raises the Yang
BL 23: Tonify Kidney
BL 25: Tonify Large Intestine.
*In this case, the patients should be in treatment taking Chinese herbal medicine from 6 to 12 months to see significant changes.
Blood Stagnation
This is a chronic problem, generally after a long period of Liver Qi stagnation or a long period of Food Stagnation or Damp Heat. It may also appear after surgeries or trauma.
SYMPTOMS
Patients have a dark complexion, lips, nails, and eyes…
Fixed and localized pain, sharp and worse with pressure
Chronic diarrhea with tenesmus may alternate with constipation, like irritable bowel syndrome IBS. The stools may be tarry.
Pulse: choppy
Tongue: purple body or purple dots, prominent dark sublingual veins.
TREATMENT PRINCIPLES
Move the blood into the intestines.
CHINESE HERBAL MEDICINE
XUE FU ZHU YU WAN
ACUPUNCTURE TREATMENT
Live 3 + Lli 4: Four gates, together they move qi and blood, eliminate stagnation, and reduce pain.
Sp 10: move blood
Sp 8: move blood in the lower jiao
Sp 6: regulates Spleen
BL17: reduces blood stagnation
Ren 6: moves Qi
St 25: Regulates Intestine
Scientific Studies Backing Chinese Medicine
There are plenty of double-blind placebo-controlled studies, randomized controlled clinical trials, and meta-analysis confirming the efficacy of Traditional Chinese Medicine, specifically Chinese herbal medicine, in treating diarrhea and irritable bowel syndrome.
For example, this PubMed Meta-Analysis of Randomized, Double-Blind, Placebo-Controlled Trials, https://pubmed.ncbi.nlm.nih.gov/27547226/
This study was made to evaluate the Chinese herbal medicine in treating diarrhea-predominant irritable bowel syndrome. They selected randomized, double-blind, and placebo-controlled trials. The data extraction was made from English and Chinese databases.
Fourteen trials from 1551 patients with IBS demonstrated that in the treatment group, there was a significant abdominal pain improvement, diarrhea improvement, and lower IBS Symptom Severity Score.
Conclusion
Traditional Chinese Medicine TCM has a long history of thousands of years of treating patients with all kinds of health problems; it has been in use way longer than western medicine; even more, significant, both are very different; they are complementary and alternative medicine like Chinese medicine together can achieve more meaningful results. Traditional Chinese medicine has proven its efficacy and safety, not only by controlled trials, systematic reviews, or double-blind placebo-controlled studies but with thousands of years of practice. Chinese medicine improves the quality of life of many patients with Chinese herbal medicine, acupuncture, moxibustion, and nutrition.
Chinese Herbal medicine is an excellent treatment for irritable bowel syndrome, diarrhea-predominant irritable bowel, abdominal pain, etc., improving the quality of life of millions of patients worldwide, being the perfect complementary and alternative medicine of western medicine.
*This article is ment to educate and not for diagnosis or treatment, alway contact your primary care provider.



Comments